Publication
Article
Optimizing Cholesterol Management: Incorporating Injectable Lipid-Lowering Therapies
Author(s):
Key Takeaways
- In 2019, 24 million US adults had ASCVD, with many not meeting LDL-C targets despite increased LLT use.
- Rural healthcare systems face challenges in managing cholesterol due to limited resources and lack of structured programs.
Challenges include therapy gaps, nonadherence, and fragmented care.
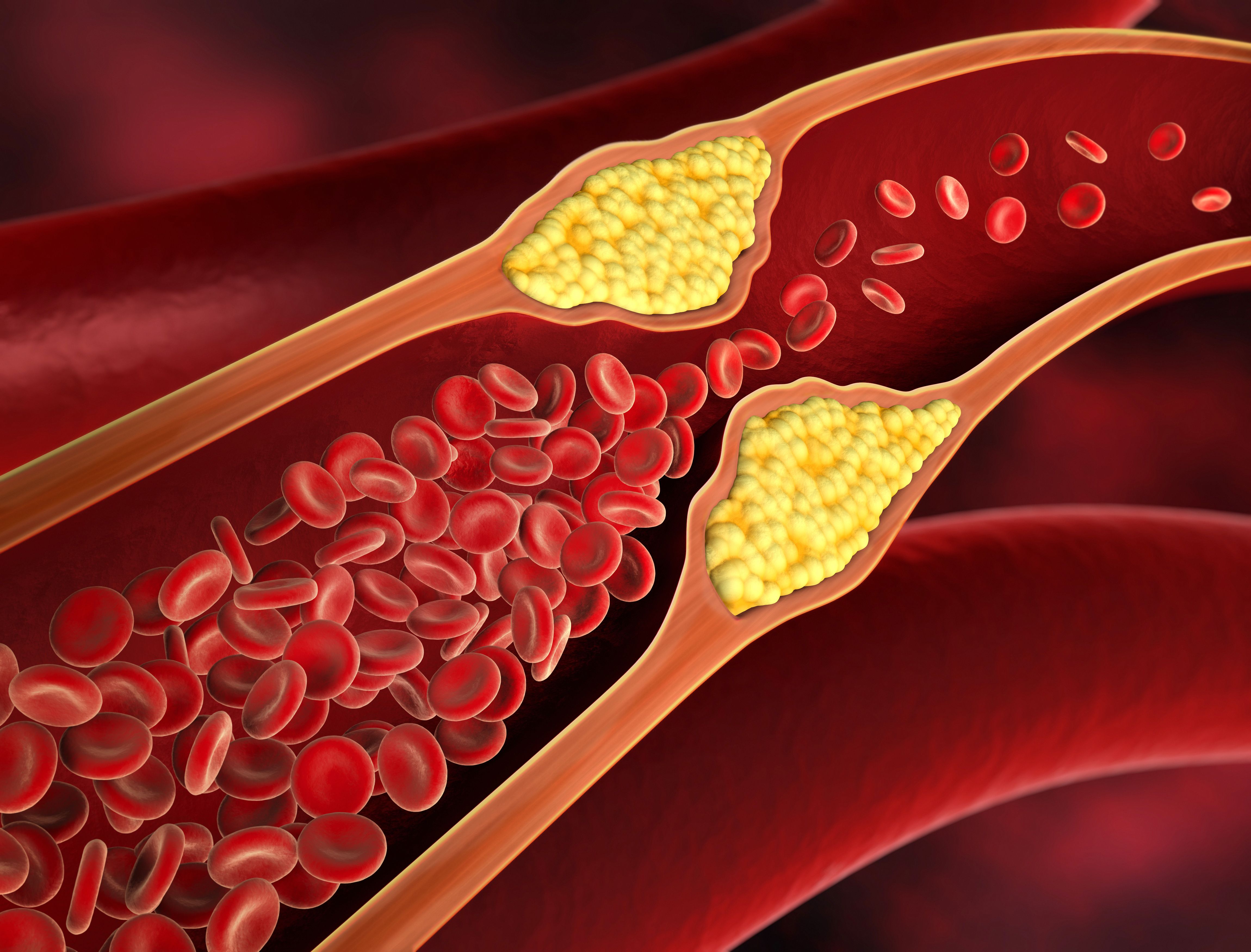
Image credit: peterschreiber.media | stock.adobe.com
In 2019, 24 million people in the US had atherosclerotic cardiovascular disease (ASCVD), which is approximately 10% of the total adult population older than 21 years. Compared with 2014, in 2019 there was a significant increase in the use of lipid-lowering therapies (LLTs), especially of high-intensity statins, in patients with ASCVD: 3.8% of patients on ezetimibe (Zetia; Merck), less than 1% on PCSK9 inhibitors, and more than 40% on no LLTs. Among patients with ASCVD, 31.2% are at very high risk for recurrent events. Further, the majority of patients with ASCVD are not at the guideline-recommended low-density lipoprotein cholesterol (LDL-C) goal.1
Unmet Needs in Managing Cholesterol in Very High-Risk Patients With ASCVD
In a Pharmacy Times Clinical Forum in Chicago, Illinois, moderated by Craig Beavers, PharmD, FAHA, BCPS-AQ Cardiology, CACP, vice president of operations and a cardiovascular clinical pharmacist at Baptist Health Paducah in Paducah, Kentucky, the panelists discussed gaps and challenges in the management of cholesterol, particularly among very high-risk patients with ASCVD. According to the panelists, these challenges are compounded in rural and regional health care systems, where resources such as pharmacy services or structured lipid management programs are often lacking. The conversation underscored the importance of ensuring adequate follow-up, adherence, and appropriate escalation of therapy to achieve guideline-directed LDL-C targets. Pharmacists in rural settings who participated in the panel discussion noted difficulties in maintaining continuity of care for patients after discharge or referral. Pharmacy services, which play a critical role in optimizing therapy, are often unavailable where patients transition, highlighting the need for a structured plan to ensure long-term follow-up and adherence to therapy goals.
“I’ll tell you, in Kentucky, where we live, and you guys probably deal with this too—so not just saying it’s a rural issue because even in a city, it can be a challenge—but we actually use a lot of inclisiran [Leqvio; Novartis Pharmaceuticals] because it is hard for our patients to get back [to our clinic] to do things, or to even get to pick certain prescriptions up,” Beavers said during the Clinical Forum.
Nonadherence remains a widespread issue, often stemming from adverse effects (AEs), lack of understanding, or insufficient follow-up, according to Beavers. Outpatient PCSK9 consult services have reported identifying significant adherence problems during chart reviews, for example. Moreover, chart reviews can help to uncover which patients are not adequately escalated to the next line of therapy (eg, ezetimibe or PCSK9 inhibitors), despite failing to meet LDL targets.
“From the outpatient perspective, at least from our PCSK9 consult service, typically the providers will put in a consult and essentially say, ‘We need to do something. We need to escalate therapy,’ but often when we do a chart review or we call the patients, we identify a ton of nonadherence for any number of reasons, whether [they have adverse] effects or they just didn’t really understand the therapies or the need for them,” explained panelist Erika Hellenbart, PharmD, BCPS, a clinical pharmacist and clinical assistant professor at University of Illinois at Chicago, during the Clinical Forum.
Inpatient vs Outpatient Gaps
According to the panelists, on the inpatient side, cholesterol management tends to focus on “checking the box” for statin therapy initiation. Augmentation of therapy—such as adding nonstatin agents such as ezetimibe or PCSK9 inhibitors—is often overlooked, especially if patients are already on a high-intensity statin. Further, physicians frequently defer lipid optimization to outpatient care without clear ownership of the transition process.
On the outpatient side, pharmacists in ambulatory care practices play a pivotal role in addressing gaps in outpatient care. With greater autonomy and the ability to provide close follow-up, pharmacists ensure appropriate escalation of therapy, improve adherence, and educate patients. However, gaps remain for patients not referred to these services, according to the panelists.
The discussion also revealed that many institutions lack robust data tracking systems or dashboards to measure how well high-risk patients with ASCVD meet LDL-C targets. During retrospective reviews, these low rates of therapy escalation can be uncovered. For instance, one center learned during a retrospective review that fewer than 50% of eligible patients received therapy intensification postevent. Without these data, it becomes challenging to identify gaps, hold the appropriate health care professionals accountable, and implement practice improvements.
Shared Decision-Making in Lipid Management
In clinical practice, shared decision-making is a vital framework for aligning treatment strategies with patient preferences, especially when considering LLTs. Panelists in the Clinical Forum emphasized the importance of treating patients holistically, which requires engaging them as individuals. While conversations about therapies can sometimes be complex, panelists shared practical approaches that facilitate patient understanding and promote informed decision-making.
For example, visual aids and simplified tools play a significant role in these educational discussions. Handouts, written explanations, and dummy pens are often employed to break down treatment plans, according to the panelists. Patients are encouraged to verbalize their understanding, ensuring clarity in navigating options such as oral medications, PCSK9 inhibitors, or emerging therapies. Despite such efforts, the panelists acknowledged that patients may retain only a fraction of the information provided, reinforcing the need for repeated engagement and simplified education.
When evaluating treatment pathways, the panelists explained that they assess the magnitude of LDL reduction required and individual preferences regarding treatment modalities, such as home-based or in-clinic injections. Although PCSK9 inhibitors (eg, evolocumab [Repatha; Amgen] and alirocumab [Praluent; Regeneron Pharmaceuticals, Inc and Sanofi]) have become more accessible, insurance requirements—such as mandatory clinical trials of ezetimibe—remain a barrier. Bempedoic acid (Nexletol; Esperion Therapeutics, Inc) was also briefly discussed as an alternative, but its approval process and formulary challenges limit widespread use, according to the panelists.
Fragmentation of care emerged as a recurring challenge as well. Physicians frequently defer responsibility among specialists, leading to missed opportunities for optimal therapy initiation and follow-up. Pharmacists, however, are uniquely positioned to bridge these gaps. Their expertise in prior authorizations (PAs), formulary navigation, and patient counseling has proven invaluable for optimizing therapy, particularly in advanced or high-risk patients with ASCVD Increased pharmacist involvement—both in the clinic and during care transitions—was highlighted as a significant opportunity for improvement.
However, the panelists noted several barriers to expanding pharmacist engagement, such as resource limitations, lack of provider time, and fragmented systems. Panelists suggested leveraging informatics and clinical decision support tools to drive standardization. Algorithm-based prompts, tied to LDL thresholds, could facilitate earlier pharmacy involvement and ensure therapy optimization. However, prioritizing informatics solutions often requires physician champions to advocate for systemic change.
Injectable LLTs
For the selection and implementation of injectable LLTs, particularly inclisiran and PCSK9 inhibitors (eg, evolocumab and alirocumab), in clinical practice, panelists explored decision-making factors such as safety, efficacy, and logistical considerations in managing these therapies for patients with persistent hyperlipidemia despite maximally tolerated statins.
Efficacy and Safety
Most panelists acknowledged the similarities between inclisiran and PCSK9 inhibitors in mechanism and LDL-lowering efficacy. However, the panelists noted some concerns about inclisiran, primarily stemming from its lack of extensive long-term cardiovascular outcomes data (beyond 2 to 3 years), though mechanistic similarities with PCSK9 inhibitors provided a degree of reassurance.
Patient Preferences and Accessibility
The group emphasized that therapy selection of injectable LLTs often depends on patient characteristics, preferences, and logistics. For example, patients who find frequent medication administration to be a challenge might benefit from inclisiran’s biannual dosing schedule. Conversely, those comfortable with self-administration at home often preferred PCSK9 inhibitors due to their flexibility. Additionally, rural or underserved populations face unique challenges, and inclisiran’s less frequent administration was seen as advantageous for patients with limited access to health care facilities.
Barriers and Implementation Challenges
PA processes emerged as a significant barrier during the discussion, especially in ambulatory settings where physicians balance multiple responsibilities. Some clinicians proactively document PA details, while others rely on dedicated teams or drug manufacturer programs to streamline renewals. Effective systems, such as automatic work queues and reminders, were highlighted as beneficial when managing ongoing therapy.
Cost and Bias Considerations
Cost remains a crucial factor in decision-making, particularly when evaluating inclisiran vs PCSK9 inhibitors under medical (buy-and-bill) or pharmacy benefits. Participants acknowledged that their own biases, such as familiarity with existing therapies or concerns about newer mechanisms such as RNA therapeutics, may unconsciously influence patient discussions. Additionally, transparency about drug mechanisms and clinical data was considered vital for patient education and decision-making.
Patient Case: JB
A case-based discussion highlighted considerations for selecting adjunctive therapy for a 64-year-old man named JB with a history of coronary artery disease, status post–myocardial infarction and stent placement 3 years ago. JB is maintained on atorvastatin (Lipitor; Pfizer) 80 mg daily. He also takes metoprolol succinate XL (Toprol XL; Melinta Therapeutics) 50 mg daily, lisinopril (Prinivil; Merck) 10 mg daily, aspirin 81 mg daily, and metformin 1000 mg twice a day. However, JB continues to have an LDL-C of 120 mg/dL and feels overwhelmed by the number of pills he’s already taking. His past medical history includes hyperlipidemia, hypertension, and type 2 diabetes (T2D). JB is physically active, and his tobacco use is 43 pack-years; he continues to smoke.
For JB, the panelists explained that they favored injectable therapies but stressed assessing patient adherence, cost, and lifestyle factors (eg, smoking cessation, diet, and exercise) before deciding. While PCSK9 inhibitors are often the default due to their robust safety data, the panelists noted that inclisiran remains an option for patients seeking less frequent dosing or with barriers to self-injection.
The panelists also generally accepted the safety and efficacy of both inclisiran and PCSK9 inhibitors while recognizing the importance of tailoring the therapy to the patient’s preferences, logistical constraints, and cost considerations.
Patient Case: DJ
The discussion also centered on optimizing the treatment of DJ, a 68-year-old female patient with multiple comorbidities, including hyperlipidemia, hypertension, T2D, stage 3 chronic kidney disease, arthritis, and limited mobility. DJ is a complex patient with coronary artery disease poststent placement 2 years ago. Six months ago, she experienced a non-ST segment elevation myocardial infarction, requiring additional stent placement. She has been maximized on rosuvastatin (Crestor; AstraZeneca) 40 mg daily. She also takes valsartan (Diovan; Novartis Pharmaceuticals) 160 mg daily, metformin 1000 mg twice a day, empagliflozin (Jardiance; Boehringer Ingelheim) 25 mg daily, aspirin 81 mg daily, and metoprolol succinate XL 50 mg daily. However, DJ continues to have an LDL cholesterol level of 110 mg/dL, blood pressure at 140/90, and hemoglobin A1c at 8.2%.
When discussing this patient case, the group emphasized the importance of first assessing medication adherence, including the use of refill histories and detailed questioning to confirm patient compliance and identify potential AEs or intolerance to statins. Addressing barriers such as perceived AEs, patient pushback, and misinformation—particularly from social media—was highlighted as a major challenge, with some patients expressing fears related to dementia or diabetes onset due to statin use.
Moving Forward: The Role of Pharmacists
The panelists concluded that pharmacists, particularly in ambulatory care and specialty roles, are key to addressing unmet needs for very high-risk patients with ASCVD. Strategies for pharmacists to address these needs include establishing lipid management consult services to streamline therapy optimization, improving transitions of care through structured handoffs, leveraging data and dashboards to measure outcomes and identify gaps, and educating providers on guideline-directed therapy escalation. Ultimately, addressing these gaps requires a concerted effort to measure performance, address gaps presented in data, and implement systems that ensure very high-risk patients with ASCVD achieve optimal cholesterol control.
The panelists also noted that pharmacists should evaluate the full medication list for deprescribing opportunities or consolidating therapies to enhance adherence. The team also discussed alternative therapies, particularly for statin-intolerant patients, and the need for robust patient follow-up and monitoring to mitigate concerns about new treatments.
System-level barriers, such as time and resource limitations and clinical inertia, were identified as key challenges by the panelists. Participants noted the importance of integrating pharmacists into specialty and primary care clinics, emphasizing comprehensive medication management protocols that address multiple chronic conditions simultaneously. The conversation highlighted the need for sustainable solutions, such as building referral pathways, improving clinic workflows, and using informatics to streamline care. Ultimately, the group underscored the pharmacist’s unique role in managing cardiovascular risks within a broader framework of chronic disease management.
REFERENCE
Gu J, Sanchez R, Chauhan A, Fazio S, Wong N. Lipid treatment status and goal attainment among patients with atherosclerotic cardiovascular disease in the United States: a 2019 update. Am J Prev Cardiol. 2022;10:100336. doi:10.1016/j.ajpc.2022.100336
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.






