News
Article
Kansas Reports Historic Numbers of Active Tuberculosis Cases
Author(s):
Key Takeaways
- Kansas reports 67 active TB cases, with health departments following CDC guidelines for testing and treatment.
- Active TB symptoms depend on infection site, with lung TB causing severe coughs and systemic symptoms.
Pharmacists can have informed discussions with patients about the importance of adherence to tuberculosis (TB) treatment regimens, especially for patients with active TB.
The Kansas Department of Health and Environment reported a historic number of active tuberculosis (TB) cases in the state, although most cases were very low-risk to the general public, including surrounding counties.1
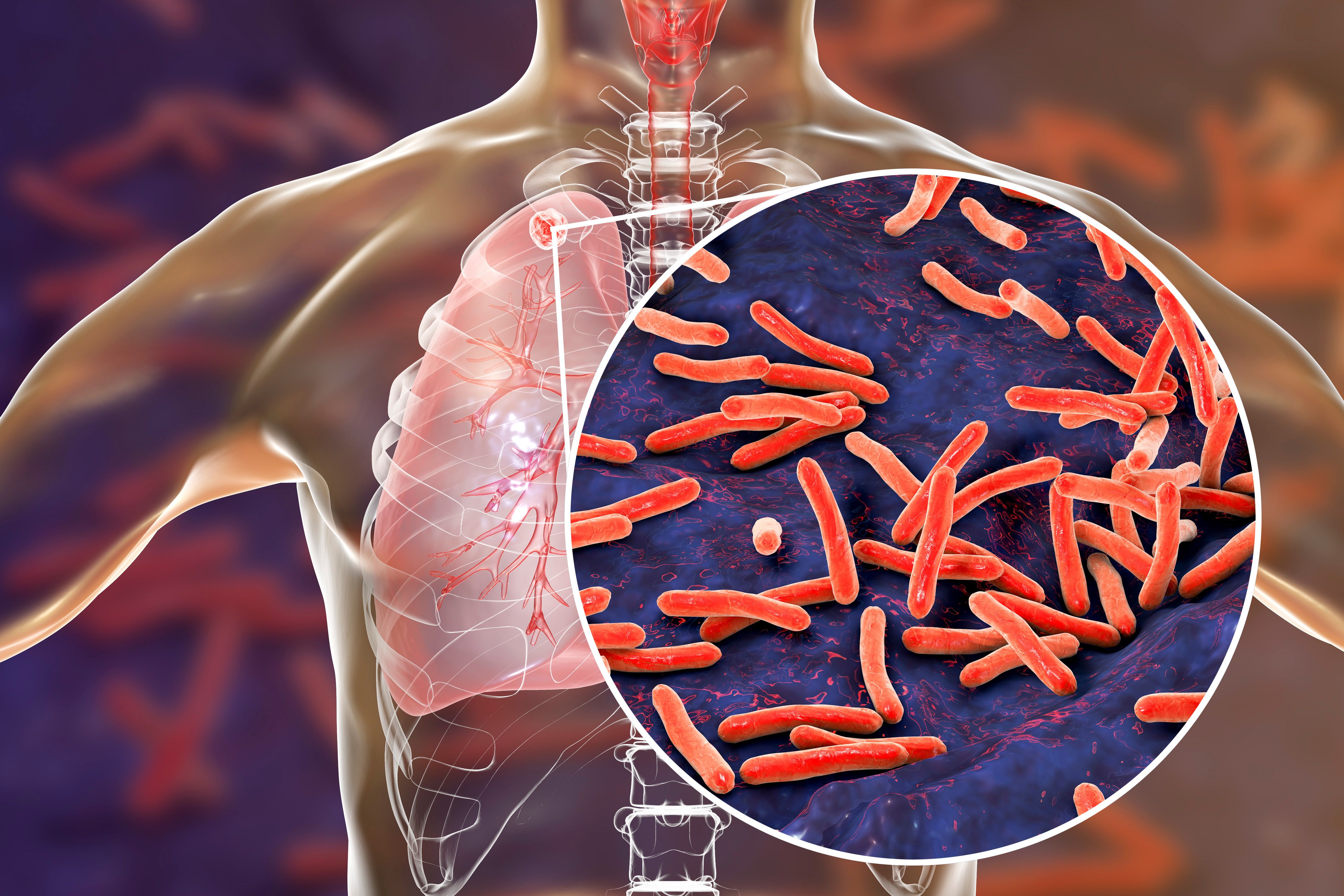
As of January 24, 2025, there have been 67 confirmed active cases in Wyandotte and Johnson counties in Kansas. | Image Credit: Dr_Microbe | stock.adobe.com
As of January 24, 2025, there have been 67 confirmed active cases across 2 counties in Kansas. As for latent cases, there are 77 in Wyandotte County and 2 in Johnson County.1
The Department is following standard practice in infectious diseases in line with the guidance of the CDC. Local health departments will conduct TB testing for patients identified as possible close contacts at no cost, and those who test positive will be further screened to determine whether TB is active or latent.1
Symptoms of active TB depend on where the bacteria are growing; usually, TB grows in the lungs. Active TB in the lungs could result in a severe cough that lasts 3 weeks or longer, pain in the chest, and coughing up blood or phlegm from deep inside the lungs, according to the CDC. Other symptoms can include weakness, fatigue, weight loss, lack of appetite, chills, fever, and night sweats. Symptoms of TB in other parts of the body can include red or purple swelling of the skin if the infection is in the lymph nodes, blood in the urine if it is in the kidneys, headache or confusion if it is in the brain, back pain if it is in the spine, or hoarseness if bacteria are in the larynx. For inactive TB, individuals may not have symptoms, but they should be treated in order to prevent active TB.2
There are a variety of treatment plans for inactive TB, including 3-, 4-, 6-, and 9-month plans, but the treatment plans typically include different combinations of medicines, including isoniazid, rifampin, and rifapentine. It is essential for patients to complete the whole regimen in order to kill all the TB bacteria; so the 3- or 4-month treatment plans are preferred, including 3 months of once-weekly isoniazid and rifapentine, 4 months of daily rifampin, or 3 months of daily isoniazid and rifampin. For active TB, regimens also include multiple medications that keep the germs from becoming treatment-resistant. Medications for active TB include ethambutol, rifampin, isoniazid, moxifloxacin, rifapentine, and pyrazinamide.3,4
The CDC recommends directly observed therapy, in which a patient will meet a health care professional every day or several times a week. The meeting can be in-person or via telehealth so that the health care provider can monitor the use of the TB medications and make sure the therapy is working properly. It is essential to take the medication as prescribed and at the same time every day.3,4
Pharmacists are an essential member of the care team to fight tuberculosis. Through accessibility and knowledge of medications, pharmacists are positioned to improve diagnosis, treatment, and patient outcomes of TB. Pharmacists can have informed discussions with patients about the importance of adherence, risks of non-treatment, and management of symptoms of TB or adverse effects of medication.5
In a study published in Healthcare (Basel), researchers said pharmacists can play 9 distinct roles in TB management and prevention, including screening, care referrals, testing, dispensing medications, engaging in directly observed therapy, counseling, reducing socioeconomic barriers, procuring medications, performing quality assurance of medications, and maintaining pharmacy data systems. They are uniquely positioned in the community to expand their roles into TB management and prevention.6
REFERENCES
1. Kansas Department of Health and Environment. Tuberculosis Outbreaks. January 24, 2025. Accessed January 28, 2025. https://www.kdhe.ks.gov/2242/Tuberculosis-Outbreaks
2. CDC. Signs and symptoms of tuberculosis. Accessed January 28, 2025. https://www.cdc.gov/tb/signs-symptoms/index.html
3. CDC. Treating inactive tuberculosis. Accessed January 28, 2025. https://www.cdc.gov/tb/treatment/inactive-tuberculosis.html
4. Commonwealth Pharmacists Association. Empowering pharmacists to be the difference in ending tuberculosis. Accessed January 28, 2025. https://commonwealthpharmacy.org/empowering-pharmacists-to-be-the-difference-in-ending-tuberculosis/
5. Cernasev A, Stillo J, Black J, Batchu M, Bell E, Tschampl CA. Pharmacists' Role in Global TB Elimination: Practices, Pitfalls, and Potential. Healthcare (Basel). 2024;12(11):1137. Published 2024 Jun 3. doi:10.3390/healthcare12111137
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.






