News
Article
Blinatumomab Plus Chemotherapy Improves DFS in Pediatric Patients With SR B-ALL
Author(s):
Key Takeaways
- Blinatumomab combined with chemotherapy significantly improved 3-year DFS in pediatric standard risk B-ALL patients, surpassing chemotherapy alone.
- The phase 3 AALL1731 trial showed blinatumomab's efficacy in reducing bone marrow relapses, particularly in SR-average and SR-high groups.
In newly diagnosed average and high standard risk B-cell acute lymphoblastic leukemia (B-ALL), blinatumomab improved disease-free survival (DFS) by approximately 97.5% and 94.1%, respectively.
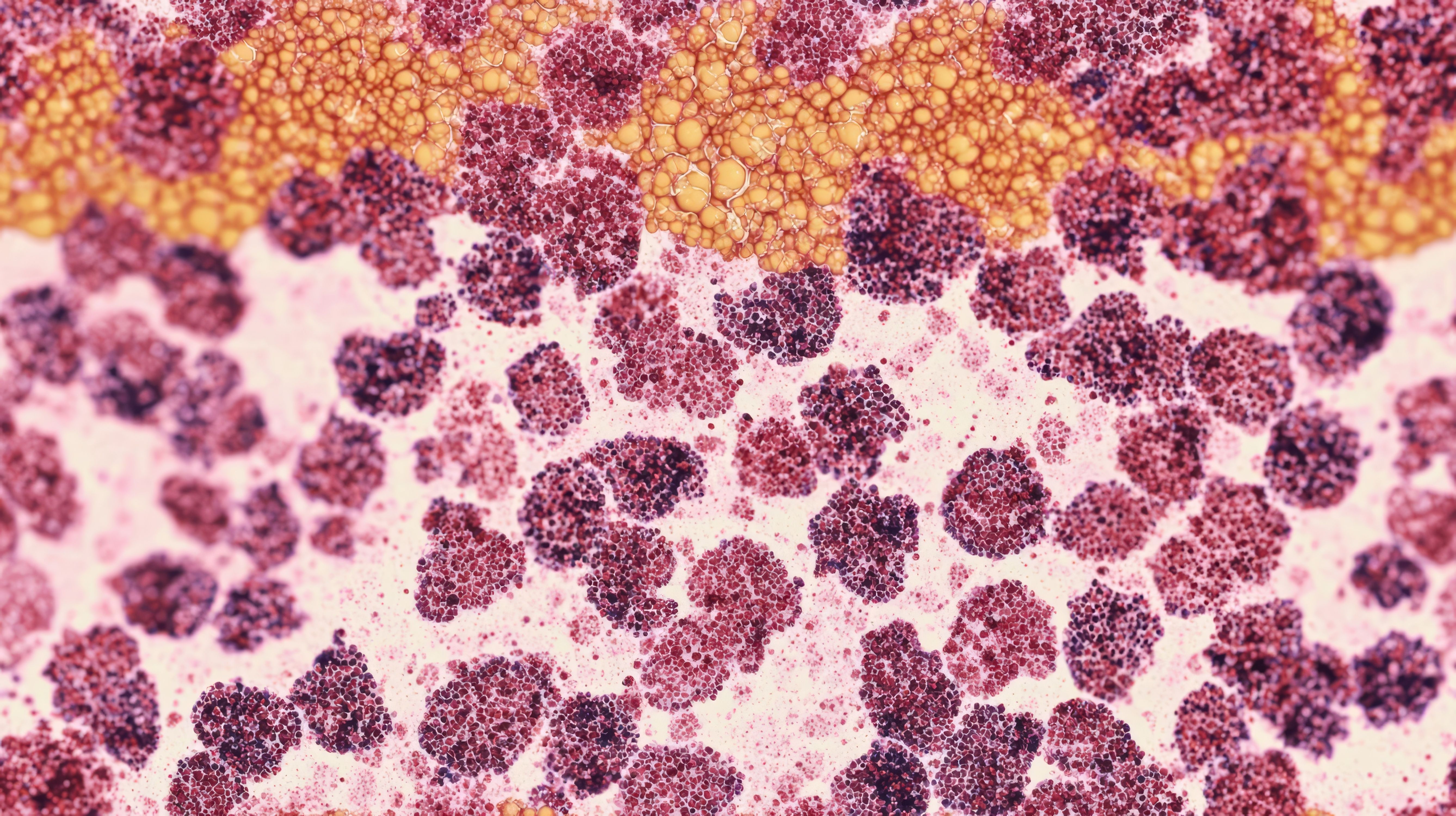
Image credit: Oleksandr | stock.adobe.com

When added to chemotherapy, blinatumomab (Blincyto; Amgen) significantly improved disease-free survival (DFS) in pediatric patients with newly diagnosed standard risk (SR) B-cell acute lymphoblastic leukemia (B-ALL), explained Rachel E. Rau, MD, of Seattle Children’s Hospital, University of Washington, in a 2024 American Society of Hematology (ASH) Annual Meeting and Exposition presentation. With these findings from the phase 3 AALL1731 clinical trial (NCT03914625), Rau noted optimism that blinatumomab with chemotherapy may represent a new treatment standard.1
According to Rau, AALL1731 was a phase 3 clinical trial which enrolled pediatric patients who were newly diagnosed with SR B-ALL, all of whom were BCR::ABL1 negative and without testicular or central nervous system (CNS)-3 disease. All participants began a standard 3-drug induction treatment prior to being assigned to 1 of 3 risk groups based on their expected risk of relapse and other factors (eg, CNS status, tumor genetics): SR-favorable (SR-fav), SR-average (SR-avg), and SR-high.1,2
Rau explained that patients with favorable cytogenetics, day 8 peripheral blood (PB) multiparameter flow cytometry (mpFC) with defined minimal residual disease (MRD) of less than 1%, and end of induction (EOI) bone marrow mpFC MRD of less than 0.01%, were categorized as SR-favorable, whereas those with unfavorable cytogenetics, EOI mpFC MRD of 0.1% or higher for double trisomies and 0.01% or higher for all others, or neutral cytogenetics with CNS2 status were categorized as SR-high. All other patients were considered SR-avg.1,2
Additionally, Rau explained that patients in the SR-fav group were known to have excellent survival with standard chemotherapy alone, and these patients were not randomly assigned and received standard treatment. Patients in the SV-avg and SV-high groups were randomly assigned if their high-throughput sequencing MRD assay scores were high (approximately 80% of patients) and end consolidation bone marrow mpFC MRD of 0.1% of less, respectively, were randomized to receive blinatumomab with their chemotherapy. These were arms B (n = 417) and D (n = 301), respectively, whereas the non-randomized groups were arms A (n = 418) and C (n = 304).1,2
“[Patients who are low MRD negative are] another group of patients with an excellent expected survival with standard chemotherapy, and they, too, were non-randomly assigned to standard treatment alone. All other standard risk average patients were eligible for our randomization,” Rau said during the ASH presentation. “A small subset of [SR-high patients] patients were still in the consolidation MRD positive, and [they] were not randomly assigned to receive chemotherapy plus blinatumomab, because at the time of trial design, limited amount was already approved for patients with an MRD above [their] threshold. All other SR-high patients were eligible for our randomization.”1
Approximately 63% (n = 1440) of the total 2245 SR-avg and SR-high eligible and evaluable patients were randomly assigned and had a median follow-up of approximately 2.5 years (IQR: 1.6-3.2 years). The median age of patients was approximately 4.3 years (IQR: 2.8-6.4 years), and most patients were boys (52.6%). Additionally, approximately 26% were Hispanic and 5% were non-Hispanic Black.1
According to Rau, intent-to-treat analyses demonstrated that the 3-year DFS was 96.0% ± 1.2% for patients randomly assigned to blinatumomab arms, compared with 87.9% ± 2.1% for those who received chemotherapy alone. The addition of blinatumomab to chemotherapy was shown to significantly improve DFS [HR 0.39, 95% CI 0.24-0.64; 1-sided P < .0001], which considerably surpassed pre-specified interim efficacy stopping criteria. Among SR-avg patients, the 3-year DFS for arm B was approximately 97.5% ± 1.3% compared with 90.2% ± 2.3% for arm A (HR 0.33, 95% CI 0.15-0.69). In addition, the SR-High patients in arm D also had better 3-year DFS, with arm D showing improvements of approximately 94.1% ± 2.5% compared with 84.8% ± 3.8% for arm C (HR 0.45, 95% CI 0.24-0.85).1
Overall, there were 6 deaths that occurred in remission, all of which were among SR-high patients (arm C: n = 2; arm D: n = 4). None occurred during blinatumomab cycles. A total of 56 relapses were observed in the control arms, with 10 being isolated CNS, 34 isolated bone marrow, and 5 a combination of CNS and bone marrow. Additionally, 19 relapses were present in the blinatumomab arms, of which 9 were isolated CNS, 9 isolated bone marrow, and 1 combined. Blinatumomab was also shown to be well tolerated, with approximately 0.3% of first courses associated with grade 3 or higher cytokine release syndrome and 0.7% with seizures.1
“When analyzed separately, we saw among SR-avg and SR-high patients [who were randomly assigned] to receive blinatumomab, they had similar improvements in DFS compared to those who received chemotherapy alone. The improvement in DFS was secondary to significant reduction in bone marrow relapses. In the overall cohort, there was a significant reduction in relapses, prominently displayed as those reductions in the relapses of the bone marrow. We did not see similar reduction in the [rarer] event of an isolated CNS relapse. This finding was not surprising, given blinatumomab’s known limited activity in the CNS,” said Rau.1
Rau emphasized that blinatumomab can represent a new treatment standard for most patients with newly diagnosed B-ALL. It can reduce instances of bone marrow relapses and was well tolerated by patients who were treated with the agent plus chemotherapy.1
REFERENCES
Rau, R. Putting Women & Children First To Optimize Their Hematology Health: Blinatumomab Added to Chemotherapy Improves Disease-Free Survival in Newly Diagnosed NCI Standard Risk Pediatric B-Acute Lymphoblastic Leukemia: Results from the Randomized Children’s Oncology Group Study AALL1731. Presented at: American Society of Hematology Annual Meeting and Exposition; San Diego, CA. December 7-10.
A Study to Investigate Blinatumomab in Combination With Chemotherapy in Patients With Newly Diagnosed B-Lymphoblastic Leukemia. ClinicalTrials.gov identifier: NCT03914625. Updated December 4, 2024. Accessed December 5, 2024. https://clinicaltrials.gov/study/NCT03914625
Newsletter
Stay informed on drug updates, treatment guidelines, and pharmacy practice trends—subscribe to Pharmacy Times for weekly clinical insights.